Introduction:
Allogeneic stem-cell transplantation (HSCT) continues to be a potentially curative approach for acute lymphoblastic leukemia (ALL). However, one of the primary challenges in HSCT remains the transplantation-related mortality (TRM), even though the overall complications and mortality rates have decreased over time. Notably, in developing countries, previous research on HSCT has highlighted that early mortality plays a significant role in their comparatively worse outcomes. Therefore, it is crucial to identify the factors involved in early mortality to enhance cure rates. Considering this, our study aims to investigate the risk factors associated with early mortality following HSCT for ALL in Brazilian centers.
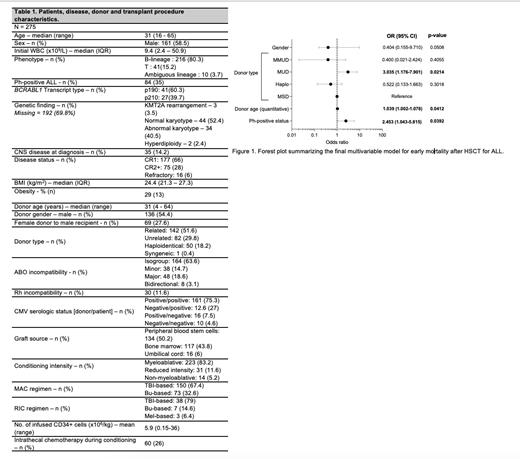
Methods: This is a retrospective registry study. Patients with ALL or ambiguous lineage leukemia above 16 years who underwent a first HSCT in 5 Brazilian centers between January 2007 and December 2017 were included. Early mortality (EM) was defined as death within 100 days from HSCT. A multivariable analysis (MVA) was performed using logistic regression, with the Akaike's information criteria used for model selection. A p-value<0.05 was considered statistically significant.
Results:
Overall, 275 patients were included in this study. Baseline characteristics are summarized in Table 1. The median age was 31y (range, 16-65) and 58.5% were male. The Philadelphia chromosome was reported in 35% and most patients were in first complete remission (CR1) (66%). Matched sibling donor (MSD), matched unrelated donor (MUD), mismatched unrelated donor (MMUD), haploidentical donor, and umbilical cord were reported in 53%, 19%, 9%, 19%, and 5%, respectively. The median donor age was 31y (range, 4-64) and 54.4% were male. EM rate was 24.4%. Univariate analysis pointed some factors statistically related to EM, as it follows: graft source (p<0.001), baseline KPS (p=0.03), gender (female vs. male, 16.7 vs 27.9%, p=0.03), Ph-positive status (p=0.03), refractory disease status (p=0.015), umbilical cord blood source (p=0.01), and donor age (p=0.08). There was no difference regarding EM rates between public and private centers (24.5 vs. 19%, p=0.463). The best multivariable model included gender, Ph-status, donor type and donor age as final variables for EM. In our cohort, Ph-positive status (OR = 2.83), donor age (OR = 1.05), and the use of MUD (OR = 3.68) were independently associated with early transplant-related mortality. Regarding the cause of EM, 69% were related to infection, and 19.5% were caused by acute GVHD. Interestingly, EM was higher in Ph-positive patients with no major molecular remission (BCR-ABL≥0.1%) - 40 vs. 3.6%, p=0.008). Cumulative incidence of acute GVHD at day 100 was 48.3% by competitive analysis. Only 3 out of 62 deaths in EM group were due to disease relapse. Remaining deaths were secondary to bacterial infection (52%), followed by acute GVHD (17.8%) and fungal infection (8.9%), mainly.
Conclusions:
This study represents the largest analysis in Brazil to assess early transplant-related mortality in ALL patients. Reducing EM rates is particularly important in resource-constrained settings to improve outcomes. While the overall patient characteristics were similar to other registry analyses, the EM rate in this study was higher than that reported in other cohorts worldwide. Notably, transplant-related factors such as donor age and type, in addition to Ph-positive status, were found to be associated with EM, outweighing previously known factors like conditioning intensity and the use of total body irradiation. These findings could aid in enhancing donor selection in Brazil and optimizing HSCT indications in specific subsets.
Disclosures
Silva:Pfizer: Honoraria; Libbs: Research Funding; Servier: Honoraria.